The measles outbreak in Disneyland is adding fuel to an already inflamed vaccine debate. Driven by a fear-based consensus orientation, the mainstream media have been flooding us with oversimplified information and hysterical headlines.
A lot of people believe that we vaccinate against measles due to its high mortality. Information presented occasionally claims a mortality rate of 3 per 1000 infected. Are such numbers reliable? There also seems to be a persistent belief that measles can be eradicated. How likely is this? It is furthermore argued that the link between MMR and autism has been disproven. What is this claim founded on?
Low mortality
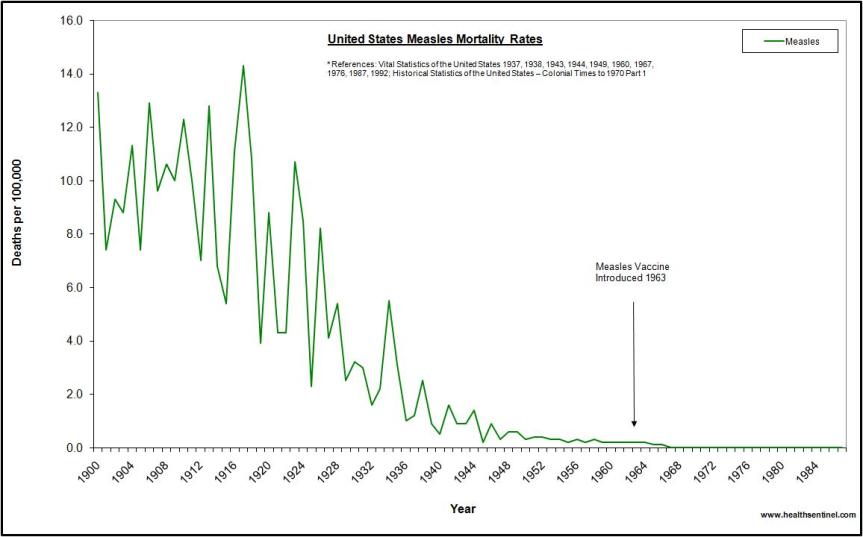
According to Dr Donald W Miller Jr (MD), the mortality rate from measles was 1 in 1 million before vaccination, and the incidence of encephalitis 1 in 100,000. The mortality rate had dropped by more than 95% before vaccination:
«With good sanitation and nutrition, the pre-vaccine mortality rate of measles in the U.S. was less than 1 in a million (compared with 14 deaths per 100,000 in 1900); seizures occurred in 1 in 3,000 people; and encephalitis, 1 in 100,000, with full recovery in 75 percent of those cases.»
«From 1900 to 1960, with improved sanitation, clean water, and better nutrition fostered by rapid delivery of fresh fruits and vegetables along with affordable refrigerators, the mortality rate from measles in the U.S. dropped more than 95 percent.»
D W Miller, Measles vs MMR vaccine: Risks and Benefits, 12.02.2015
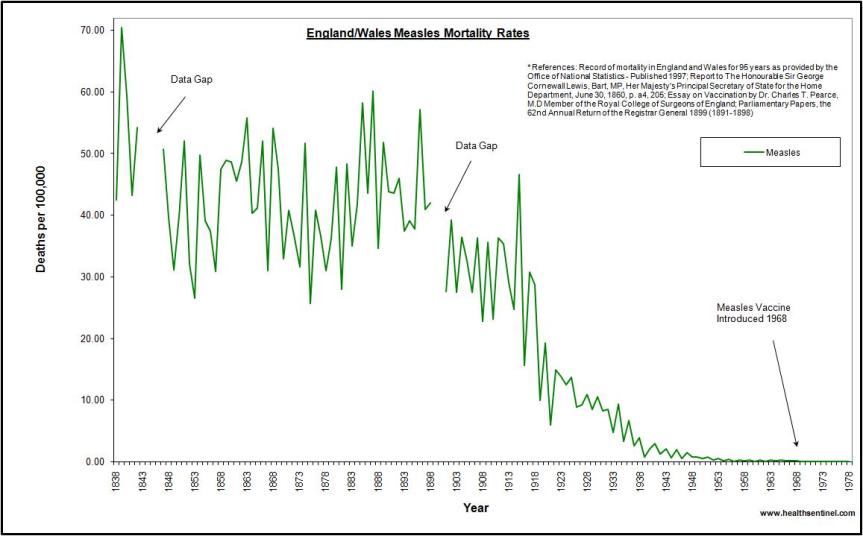
The mortality rates from England between 1993 and 2013 is low. In approximately 96.500 reported cases, 3 died as a result of acute measles infection. One was medically immunosuppressed, one had congenital immunologic disease and were unvaccinated, and the last case had a complicated outcome from pneumonia. The rest stems from measles acquired on an earlier date. Mortality from reported cases is at this basis 1 in 30,000. According to the figures mortality has decreased by 98,5% since 1940. In the pre vaccination era we can notice a decrease in mortality by 90% between 1940 and 1963.
«Prior to 2006, the last death from acute measles was in 1992. In 2006, there was 1 measles death in a 13-year-old male who had an underlying lung condition and was taking immunosuppressive drugs. Another death in 2008 was also due to acute measles in an unvaccinated child with a congenital immunodeficiency, whose condition did not require treatment with immunoglobulin.
In 2013, 1 death was reported in a 25-year-old man following acute pneumonia as a complication of measles. All other measles deaths since 1992 shown above are in older individuals and were caused by the late effects of measles. These infections were acquired during the 1980s or earlier, when epidemics of measles occurred.»
Public Health England, Measles Notifications and deaths in England and Wales: 1940-2013, GOV.UK, 10.01.2014
Probability of eradication
This discussion pertains to the WHO’s declared goal of eradicating measles and whether it is in fact possible to eradicate measles in the long term. Considering the problems related to short-term vaccine-related immunity and infection from the newly vaccinated, eradication seems unlikely to achieve. Some researchers believe it is impossible to eradicate measles, and according to Dr Levy`s calculations, measles cases will increase towards 2050.
«However, despite short-term success in eliminating the disease, long-range projections demonstrate that the proportion of susceptibles in the year 2050 may be greater than in the prevaccine era. Present vaccine technology and public health policy must be altered to deal with this eventuality.»
D. L. Levy The future of measles in highly immunized populations a modeling approach, American journal of epidemiology, Jun 1983
A segment of the population still has lifelong immunity from natural measles infection, but this applies mainly to people over the age of 40. What happens when the numbers of this naturally immune segment of the population are reduced? Will the weaker vaccine-immunity be sufficient to maintain herd immunity? How frequently do we have to vaccinate? Outbreaks of measles in fully vaccinated population have repeatedly been observed. It is a fact that vaccine-related immunity cannot compete with natural immunity.
«Outbreak of measles in a highly vaccinated secondary school population: Eighty-seven laboratory-confirmed or clinically confirmed cases of measles were identified (for an attack rate of 7.7%). The measles vaccination rate was 94.2%”
P A Sutcliffe and E Rea, Outbreake of measles in a highly vaccinated secondary school population, CMAJ JAMC, Nov 1996.
“Mild measles and secondary vaccine failure during a sustained outbreak in a highly vaccinated population.”
Edmonson MB et al, Mild measles and secondary vaccine failure during a sustained outbreake in highly vaccinated population, Journal of The American Medical Association, May 1990
“During the Spring of 1978, students with a history of previous measles vaccination accounted for over three-forths of 203 cases of measles in a metropolitan county. Seventy cases occurred in two schools where 99% of the students were vaccinated”
R G Judelsom et al, School-based measles outbreake: correlation of age at immunization with risk og disease, American Public Health Association, Nov 1980
“We conclude that outbreaks of measles can occur in secondary schools, even when more than 99 percent of the students have been vaccinated and more than 95 percent are immune.
T L Gustafson et al, Measle outbreake in fully immunized secondary-school population, The New England Journal of Medicine, Mar 1987
“During a measles outbreak in Northern Ireland (between October 1988 and March 1989) it was noted that a proportion of cases had occurred in children who had previously been vaccinated against measles. A study was, therefore, set up to provide a rapid estimate of vaccine efficacy. Investigation of the computerised records at 31 December 1991 revealed that 94% of children in the study cohort had received measles vaccine.”
V K Tohani and F D Kennedy, Vaccine efficacy in a measles immunisation programme, Communciable disease report. CDC review, Apr 1992
“specific IgM antibodies were detected in the acute phase serum of only 30 (66.6%), of whom 17 were vaccinated. When the convalescent sera were tested, specific IgM antibodies were detected in 25 of the 28 (89.2%) vaccinated,”
L Sekla et al, An evaluation of measles serodiagnosis during an outbreak in a vaccinated community, Clinical and Investive Medicine, Aug 1988
«The index case had two doses of measles-containing vaccine. Of 88 contacts, four secondary cases were confirmed that had either two doses of measles-containing vaccine or a past positive measles IgG antibody. All cases had laboratory confirmation of measles infection, clinical symptoms consistent with measles, and high avidity IgG antibody characteristic of a secondary immune response.»
J B Rosen et al, Outbreak of measles among persons with prior evidence of immunity, New York city 2011, Clinical infectious diseases, Oxford Journals, 10.04.2014
Infection from newly vaccinated
Alongside questions about attenuated vaccine immunity, there are studies referring to viral shedding from persons recently vaccinated with live virus. This is obviously relevant when estimating the probability of success in combating the disease.
«Analysis of urine specimens by using reverse transcriptase-PCR was evaluated as a rapid assay to identify individuals infected with measles virus. For the study, daily urine samples were obtained from either 15-month-old children or young adults following measles immunization. Overall, measles virus RNA was detected in 10 of 12 children during the 2-week sampling period. In some cases, measles virus RNA was detected as early as 1 day or as late as 14 days after vaccination. Measles virus RNA was also detected in the urine samples from all four of the young adults between 1 and 13 days after vaccination. This assay will enable continued studies of the shedding and transmission of measles virus and, it is hoped, will provide a rapid means to identify measles infection, especially in mild or asymptomatic cases.»
P A Rota et al, Detection of measles virus RNA in urine specimens from vaccine recipients, Journal of Clinical Microbiology, Sept 1995.
«In the midst of a local measles outbreak, a recently immunized child was investigated for a new-onset measles-type rash. Nucleic acid testing identified that a vaccine-type measles virus was being shed in the urine. Clinically differentiating measles from a nonmeasles rash is challenging, but can be supported by a thorough medical history evaluation. Rashes are expected to occur after immunization; nucleic acid testing can be used when it is difficult to differentiate between wild and attenuated strains.»
L Nestibo et al, Differentiating the wild from the attenuated during a measle outbreak, Paediatrics and Child Health, Apr 2012.
«We describe excretion of measles vaccine strain Schwarz in a child who developed a febrile rash illness eight days after primary immunisation against measles, mumps and rubella. Throat swabs and urine specimens were collected on the fifth and sixth day of illness, respectively. Genotyping demonstrated measles vaccine strain Schwarz (genotype A). If measles and rubella were not under enhanced surveillance in Croatia, the case would have been either misreported as rubella or not recognised at all»
B Kaic et al, Spotlight on measles 2010: excretion of vaccine strain measles virus in urine and pharyngeal secretions of a child with vaccine associated febrile rash illness, Croatia, March 2010. Croatian Institute of Public Health, Department of Infectious Disease Epidemiology, Zagreb, Croatia. Eurosurveillance, 02.09.2010
«We describe a case of vaccine-associated measles in a two-year-old patient from British Columbia, Canada, in October 2013, who received her first dose of measles-containing vaccine 37 days prior to onset of prodromal symptoms. Identification of this delayed vaccine-associated case occurred in the context of an outbreak investigation of a measles cluster.»
M Murti et al, Case of vaccine-associated measles five weeks post-immunisation, Eurosurveillance, 05.12.2013
«Scientific evidence demonstrates that individuals vaccinated with live virus vaccines such as MMR (measles, mumps and rubella), rotavirus, chicken pox, shingles and influenza can shed the virus for many weeks or months afterwards and infect the vaccinated and unvaccinated alike. Furthermore, vaccine recipients can carry diseases in the back of their throat and infect others while displaying no symptoms of a disease.»
Weston A Price foundation, Studies show that vaccinated individuals spread disease, Globe Newswire, 02.02.2015.
«Dr. Suzanne Humphries is a practicing nephrologist (kidney physician). In this lecture (video below), she addresses a study done in Croatia [1] where a child who was vaccinated with the MMR vaccine was tested positive for the measles vaccine strain Schwarz eight days after vaccination.»
S Humphries, Dr. Suzanne Humperies MD – Vaccine strain in measles virus found in measles outbreaks, Vaccine impact, 11.02.2015.
In a vaccinated society, infants become more vulnerable, and it is precisely this group which needs protection. Infants were previously protected by immunity from their mothers who had undergone measles infection naturally, due to the passive immunity transferred during pregnancy and lactation. Normally children got measles around 4-9 years of age. Studies have compared immune levels between children from vaccinated and naturally immune mothers, and it turns out that mothers with natural immunity give their children better and longer immunity.
«Lower measles antibody titres were observed in children whose mothers had been vaccinated, and these decayed to undetectable values earlier than in children whose mothers had not been vaccinated, and were assumed to have had natural measles.»
P J Jenks et al, Maternally derived measles immunity in children of naturally infected and vaccinated mothers, Epidemiology and Infection, Oct 1988.
«Children of mothers vaccinated against measles and, possibly, rubella have lower concentrations of maternal antibodies and lose protection by maternal antibodies at an earlier age than children of mothers in communities that oppose vaccination. This increases the risk of disease transmission in highly vaccinated populations»
S Waaijenborg et al, Waning of meternal antibodies against measles, mumps, rubella, and varicella in communities with contrasting vaccination coverage, The journal of infectious diseases, Oxford Journals, 29.05.2013
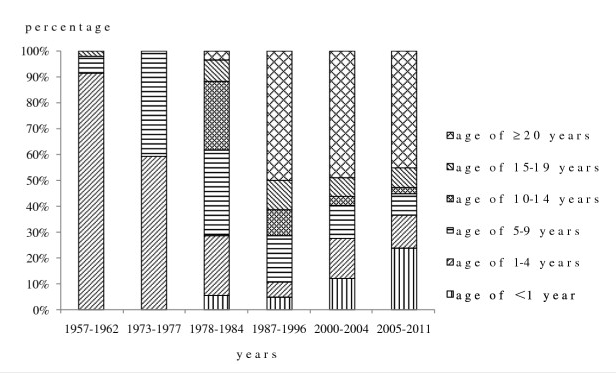
Age displacement is evident in statistics from Beijing between 1957 and 2011. They show how measles now have shifted to new vulnerable age groups like infants under 1 year of age, and this trend is increasing. It also emerges how adults more frequently are affected, but it’s questionable if this is due to the benefit of vaccines durability in an immunological perspective. Immunization coverage in Beijing is 95-99%, in other words – it is optimal.
Juan Le et al, A 60 year review on the changing epidemiology of measles in capital Beijing, China, 1951-2011, BMC Public Health, 21.10.2013.
Mumps is also a component in the MMR vaccine. In recent years we have seen an age shift in mumps infection. During several outbreaks vaccinated post pubertal men have become infected.This is unfortunate, as it’s precisely this group the vaccine is meant to protect due to danger of testicular inflammation with potential for sterility. Previously mumps were primarily a disease affecting children.
«Nearly 6,600 people became sick with the mumps, mostly in eight Midwest states including Nebraska, and the hardest-hit group was college students ages 18 to 24. Of those in that group who knew whether they had been vaccinated, 84 percent had had two mumps shots, according to the study by the Centers for Disease Control and Prevention and state health departments.»
Does mumps vaccine fade by college years, CBSNEWS, 09.04.2008
«From June 28, 2009, through June 27, 2010, a total of 3502 outbreak-related cases of mumps were reported in New York City, two upstate New York counties, and one New Jersey county. Of the 1648 cases for which clinical specimens were available, 50% were laboratory-confirmed. Orthodox Jewish persons accounted for 97% of case patients. Adolescents 13 to 17 years of age (27% of all patients) and males (78% of patients in that age group) were disproportionately affected. Among case patients 13 to 17 years of age with documented vaccination status, 89% had previously received two doses of a mumps-containing vaccine, and 8% had received one dose.»
A E Barskey, Mumps outbreak in orthodox jewish community in United States, The new England Journal of Medicine, 01.11.2012.
Saturation point
Questions have been raised about the increasing number of vaccines children are subjected to. In the US, where infants receive the most vaccines in the world, we also find a higher infant mortality rate compared to countries that vaccinate more moderately, but with otherwise similar upbringing. In most areas of life, there is a saturation point and this also applies to vaccines.
«Despite having one of the most aggressive vaccination policies in the developed world, specifying 22 vaccine doses for a total of 12 diseases by 1 year of age, the United States had higher infant mortality rates in 2009 than 33 other nations.»
E Mumper, Can awareness of medical pathophysiology in autism lead to primary care autism prevention strategies?, The North American Journal of Medicine and Science, 25.07.2013.
MMR – neurological autoimmune disorders and autism
The neurological adverse effects of the MMR vaccine also need to be discussed. Strong research indicates that the vaccine can cause autism. Some argue that the debate ended with the Wakefield case. He was the first to identify a possible association between the MMR vaccine and autism. He examined children with combined regressive autism and bowel pathology with a symptomatic onset after the MMR. The findings were dismissed in general meta studies. These studies did however not take into account the specific group with regressive autism. The effects are obviously not reflected in a corresponding degree when comparing patients with autism without a corresponding etiology. Autism may also be related to genetics, birth injuries, meningitis, encephalitis, trauma and various other factors. Regressive autism differs from other forms of autism by its sudden occurrence in a child who has exhibited normal development in the past. This happens frequently around the age of 18 months, at the same age as the first MMR injection.
Various research papers have looked at a possible link between autism and autoimmunity against CNS (Central Nervous System, respectively the brain) in combination with specific vaccine antibodies. It can be assumed that some children have an inherited or congenital vulnerability of developing such autoimmunity.
Some studies have shown that the immunization of children before 12 months of age has been problematic because of maternal antibodies. Such immunity is decreasing after birth, but it is much stronger in mothers who have undergone natural measles. Essentially, a lack of immunological response has been noted after vaccination. In addition, it can also be argued that – based on general understanding of immunology and autoimmunity – hypersensitivity and cross-reactions may occur.
The researcher V.T. Singh has contributed to a number of research papers addressing MMR and autism from an autoimmune perspective. His research is credible and shows convincing findings. It is important to emphasise that he examined the relationship between specific MMR antibodies coupled with autoimmunity related to the CNS. A few papers claimed that they could not support his findings, but these studies were limited to MMR antibodies, and not the combination of CNS-antibodies, which is the core of Singh`s research. His findings are for this reason not disapproved.
«ELISA analysis showed a significant increase in the level of MMR antibodies in autistic children. Immunoblotting analysis revealed the presence of an unusual MMR antibody in 75 of 125 (60%) autistic sera but not in control sera. This antibody specifically detected a protein of 73-75 kD of MMR. This protein band, as analyzed with monoclonal antibodies, was immunopositive for measles hemagglutinin (HA) protein but not for measles nucleoprotein and rubella or mumps viral proteins. Thus the MMR antibody in autistic sera detected measles HA protein, which is unique to the measles subunit of the vaccine. Furthermore, over 90% of MMR antibody-positive autistic sera were also positive for MBP autoantibodies, suggesting a strong association between MMR and CNS autoimmunity in autism. Stemming from this evidence, we suggest that an inappropriate antibody response to MMR, specifically the measles component thereof, might be related to pathogenesis of autism.»
V K Singh et al, Abnormal measles-mumps-rubella antibodies and CNS autoimmunity in children with autism, Journal of biomedical science, Jul-Aug 2002.
«Autoimmunity was demonstrated by the presence of brain autoantibodies, abnormal viral serology, brain and viral antibodies in CSF, a positive correlation between brain autoantibodies and viral serology, elevated levels of proinflammatory cytokines and acute-phase reactants, and a positive response to immunotherapy. Many autistic children harbored brain myelin basic protein autoantibodies and elevated levels of antibodies to measles virus and measles-mumps-rubella (MMR) vaccine. Measles might be etiologically linked to autism because measles and MMR antibodies (a viral marker) correlated positively to brain autoantibodies (an autoimmune marker)–salient features that characterize autoimmune pathology in autism. Autistic children also showed elevated levels of acute-phase reactants–a marker of systemic inflammation.
The scientific evidence is quite credible for our autoimmune hypothesis, leading to the identification of autoimmune autistic disorder (AAD) as a major subset of autism. AAD can be identified by immune tests to determine immune problems before administering immunotherapy. The author has advanced a speculative neuroautoimmune (NAI) model for autism, in which virus-induced autoimmunity is a key player. The latter should be targeted by immunotherapy to help children with autism.»
V K Singh, Phenotypic expression autoimmune autistic disorder (AAD): and major subset of autism, Annals of clinical psychiatry, Jul-Sep, 2009.
«The antibody to this antigen was found in 83% of autistic children but not in normal children or siblings of autistic children. Thus autistic children have a hyperimmune response to measles virus, which in the absence of a wild type of measles infection might be a sign of an abnormal immune reaction to the vaccine strain or virus reactivation.»
V K Singh and R L Jensen, Elevated levels of measles antibodies in children with autism, Pediatric neurology, Apr 2003.
«Considering an autoimmunity and autism connection, brain autoantibodies to myelin basic protein (anti-MBP) and neuron-axon filament protein (anti-NAFP) have been found in autistic children. In this current study, we examined associations between virus serology and autoantibody by simultaneous analysis of measles virus antibody (measles-IgG), human herpesvirus-6 antibody (HHV-6-IgG), anti-MBP, and anti-NAFP. We found that measles-IgG and HHV-6-IgG titers were moderately higher in autistic children but they did not significantly differ from normal controls. Moreover, we found that a vast majority of virus serology-positive autistic sera was also positive for brain autoantibody: (i) 90% of measles-IgG-positive autistic sera was also positive for anti-MBP; (ii) 73% of measles-IgG-positive autistic sera was also positive for anti-NAFP; (iii) 84% of HHV-6-IgG-positive autistic sera was also positive for anti-MBP; and (iv) 72% of HHV-6-IgG-positive autistic sera was also positive for anti-NAFP. This study is the first to report an association between virus serology and brain autoantibody in autism; it supports the hypothesis that a virus-induced autoimmune response may play a causal role in autism.»
V K Singh, S X Lin and V C Yang, Serological association of measles virus and herpesvirus-6 with brain autoantibodies in autism, Clinical immunology and immunophatology, Oct 1998.
CDC hiding association of MMR and autism
Last fall it was revealed that the CDC`s own research may have been subject to fraud. An association was found between autism and MMR in some groups. According to Dr. William Thompson and Dr. Brian Hooker, this information was deliberately withheld by the CDC.
«And now Dr. William Thompson, a CDC employee-researcher, has come forward recently as a whistleblower, revealing the fact that the CDC has been hiding the truth about vaccine dangers from the public, specifically with regard to MMR vaccine-induced autism. Like an Edward Snowden in the CDC, he has revealed to Dr. Brian Hooker (the Glenn Greenwald of the piece) that the CDC has committed scientific fraud. This occurred in a 2004 paper published in the journal Pediatrics, written by Dr. Thompson and other CDC employees, which hid the finding that the MMR vaccine had caused a 340 percent increased risk of autism in African-American babies. Dr. Hooker revealed this in a 2014 paper published in the journal Translational Neurodegeneration. But typical of the censorship and suppression practiced in today’s medical police state, it forced the editor of that journal to apologize for publishing this paper and retract it (as has been the case with other studies implicating MMR vaccine with autism, notably one by Dr. Andrew Wakefield published in Lancet in 1998). But in a recent development, the President has granted Dr. Thompson “Official Whistleblower Status and Immunity” to testify before Congress»
D W Miller, Measles vs MMR vaccine: Risks and Benefits, 12.02.2015
Dr Brian Hooker about CDC, vaccines and autism
Conclusion
During the twentieth century measles mortality has declined by almost 100%, where the most extensive effect originates in the pre-vaccine era.
Based on the factors such as the difference in genotypes, the highly contagious nature of measles, reduced natural immunity, inadequate vaccine immunity and potential infection from newly vaccinated, it can be argued that measles is probably impossible to eradicate. This is also supported by the fact that measles outbreaks continue to occur in highly vaccinated populations. We have seen that mathematical calculations show that measles will escalate around the year 2050. At this point, people over the age of 40 still have natural immunity due to natural measles in their childhood. The vaccine is incapable of conferring similar life-long immunity, either in individuals or in groups. Herd immunity is bound to decline when this part of the population is further reduced. The Disneyland epidemic shows that fully vaccinated and infants were also infected. Due to the reduced passive immunity from vaccinated mothers, infants are now becoming a vulnerable group. Age displacement of mumps infection to grown men is creating another at-risk group. Both groups vulnerability is related to age displacement, and must be considered a direct consequence of vaccination.
There are credible research papers which show a possible link between MMR and autoimmunity related to the central nervous system and autism. Despite claims that the science has been settled, the research has not been disproved. Lately it has emerged that the CDC’s own research paper from 2004 found an association between the MMR and autism. This information has been withheld. The accusation comes from one of CDC`s own researchers. It appears that the MMR – autism discussion has reached a new level of controversy – in spite of the mainstream media blackout.
Further information can be found at:
Dr Donald W Miller jr. MD. Article: «Measles vs MMR: risks and benefits» 12.02.2015
Dr Robert J Rowen MD. Notes: «Measles spred by the vaccinated. Vaccines may be a greater danger than you ever knew» 31.01.2015
Dr Suzanne Humphries MD. Article: «Vaccine strain of measles vaccine found i measles outbreak» 11.02.2015
B L Fisher, Report. «The emerging risk of live virus & virus vectored vaccines: Vaccine strain virus infection, shedding and transmission», The National Vaccine Information Center, 2014.
Sources:
Public Health Enland, Measles Notifications and deaths in Enland and Wales: 1940-2013, GOV.UK, 10.01.2014
D. L. Levy The future og measles in highly immunized populations a modeling approach, American journal of epidemiology, Jun 1983
P A Sutcliffe and E Rea, Outbrake of measles in a highly vaccinated secondary school population, CMAJ JAMC, Nov 1996.
Edmonson MB et al, Mild measles and secondary vaccine failure during a sustained outbrake in highly vaccinated population, Journal of The American Medical Association, May 1990.
R G Judelsom et al, School-based measles outbrakes: correlation of age at immunization with risk of disease, American Public Health Association, nov 1980.
T L Gustafson et al, Measle outbrake in fully immunized secondary-school population, The New England Journal of Medicine, Mar 1987.
V K Tohani and F D Kennedy, Vaccine efficacy in a measles immunisation programme, Communciable disease report. CDC review, Apr 1992.
L Sekla et al, An evaluation of measles serodiagnosis during an outbreak in a vaccinated community,Clinical and Investive Medicine, Aug 1988
J B Rosen et al, Outbreak of measles among persons with prior evidence of immunity, New York city 2011, Clinical infectious diseases, Oxford Journals, 10.04.2014.
P A Rota et al, Detection of measles virus RNA in urin specimens from vaccine recipients, Journal of Clinical Microbiology, Sept 1995.
L Nestibo et al, Differentiating the wild from the attenuated during a measle outbreak, Paediatrics and Child Health, Apr 2012.
B Kaic et al, Spotlight on measles 2010: excretion of vaccine strain measles virus in urine and pharyngeal secretions of a child with vaccine associated febrile rash illness, Croatia, March 2010. Croatian Institute of Public Health, Department of Infectious Disease Epidemiology, Zagreb, Croatia. Eurosurveillance, 02.09.2010
M Murti et al, Case of vaccine-associated measles five weeks post-immunisation, Eurosurveillance, 05.12.2013
Weston A Price foundation, Studies show that vaccinated individuals spread disease, Globe Newswire, 02.02.2015
S Humphries, Dr. Suzanne Humperies MD – Vaccine strain in measles virus found in measles outbreaks, Vaccine impact, 11.02.2015
P J Jenks et al, Maternally derived measles immunity in children of naturally infected and vaccinated mothers, Epidemiology and Infection, Okt 1988.
S Waaijenborg et al, Waning of metarnal antibodies against measles, mumps, rubella, and varicella in communities with contrasting vaccination coverage, The journal of infectious diseases, Oxford Journals, 2013
Juan Le et al, A 60 year review on the changing epidemiology og measles in capital Beijing, China, 1951-2011, BMC Public Health, 2013.
Does mumps vaccine fade by college years, CBSNEWS, 09.04.2008.
A E Barskey, Mumps outbreak in orthodox jewish community in United States, The new England Journal of Medicine, 01.11.2012.
E Mumper, Can awareness of medical phatophysiology in autism lead to primary care autism prevention strategies?, The North American Journal of Medicine and Science, 29.05.2013.
R M Zinkernagel, Maternal antibodies, Childhood infections, and Autoimmune disease, The New England Journal of Medicine, 01.11.2001.
V K Singh et al, Abnormal measles-mumps-rubella antibodies and CNS autoimmunity in children with autism, Journal of biomedical science, Jul-Aug 2002
V K Singh, Phenotypic expression autoimmune autistic disorder (AAD): and major subset of autism, Annals of clinical psychiatry, Jul-Sep 2009.
V K Singh and R L Jensen, Elevated levels of measles antibodies in children with autism, Pediatric neurology, Apr 2003.
V K Singh, S X Lin and V C Yang, Serological association of measles virus and herpesvirus-6 with brain autoantibodies in autism, Clinical immunology and immunophatology, Okt 1998.
Dr Donald W Miller jr. MD. Article: «Measles vs MMR: risks and benefits» 12.02.2015
Dr Robert J Rowen MD. Notes: «Measles spred by the vaccinated. Vaccines may be a greater danger than you ever knew» 31.01.2015
Dr Suzanne Humphries MD. Article: «Vaccine strain of measles vaccine found i measles outbreak» 11.02.2015